By Janice Harvey, RPh, CDE
The simple answer to this question is that PharmaCare doesn’t cover all your medication costs, even if you have special authority. But let’s start at the beginning.
HOW PHARMACARE WORKS
Every resident of British Columbia can qualify for provincial coverage. There are a number of coverage programs under PharmaCare, but the most common is Fair PharmaCare. Registration for Fair PharmaCare is not automatic. You can register online or by phone. Further details about Fair PharmaCare and how to get registered for it can be found here.
Once you are registered for Fair PharmaCare, you will have a “family deductible” and a “family maximum” that are based on your income level. For low-income families, these amounts will be less than they would be for someone in a higher income bracket. You can find out these amounts by calling PharmaCare at 1-800-663-7100.
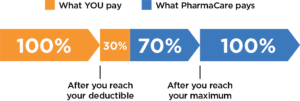
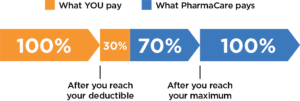
Fair PharmaCare requires that you pay the full cost of your eligible medications until you reach your deductible, at which point they will pay 70% of eligible drug costs. Once you have reached your family maximum, then they will pay 100% of those costs. For working individuals with minimal medication expenses, it is possible that PharmaCare will not end up paying for any drug costs. For individuals with many medications, coverage may kick in earlier in the year. The coverage is reset each year, so the amounts can change each January 1, depending on changes in income levels.
Only certain drugs are eligible for payment. You can use the online formulary search to see if a medication is covered as a regular benefit or if special authority is required. In some cases, a medication may not be covered at all. For drugs that are not eligible for coverage, the amount you pay will not count towards either the deductible or the maximum amount.
HOW TO APPLY FOR SPECIAL AUTHORITY
Some prescription drugs are considered “limited coverage” drugs. In other words, coverage is available, but only if specific conditions are met. Your doctor will need to apply to PharmaCare for Special Authority on your behalf and will receive a fax indicating whether or not the request has been approved. Not every request will be approved. In some cases, coverage will be approved for only a specific amount of time (e.g., 6 months), but it could also be indefinite (for as long as you take the medication).
| Pharmacists in community pharmacies will soon be able to submit Special Authority requests online, which should allow for a much faster response. Stay tuned! We will let you know as soon as that functionality is in place. |
If you have signed up for Health Gateway, you will be able to see a list of any Special Authority requests that have been submitted and whether they have been approved. While there, you can also view other health records, including lab tests, medications taken since 1995, health visits, immunizations and proof of vaccination.
ONCE YOU HAVE APPROVAL
Assuming the request is approved, your pharmacy can then process the prescription through Fair PharmaCare. If you have met your deductible under Fair Pharmacare, then 70% of the cost will be covered, or 100% if you have paid up to your maximum amount. Keep in mind, however, that at the beginning of the year it is unlikely that you have already met your deductible, so while the cost will count towards your deductible, it could be that none of the cost is covered at this time.
If you are fortunate enough to have a high income, it is entirely possible that the drug cost will not be covered at all by Fair PharmaCare, even with Special Authority in place. If you have third-party insurance through your employer or as part of a retirement package (e.g., Sunlife, Blue Cross), these plans will usually cover medications for which you have Special Authority, and your pharmacy will ensure that the drug cost is passed along to your plan whenever possible.
IT’S COMPLICATED
To keep this article relatively short, we have kept things simple. There are many exceptions to PharmaCare billing — too many to discuss here. If you would like to learn more about PharmaCare coverage policies and how they decide which drugs to cover, please visit the BC PharmaCare website.
